covid_19_training_tool_v3_01.05.2021_508
-
Upload
-
0
-
Embed
-
Share
-
Upload and view presentations on any device and embed the player to your website! --- > >Upload PPT
- Upload PPT
Presentation Transcript
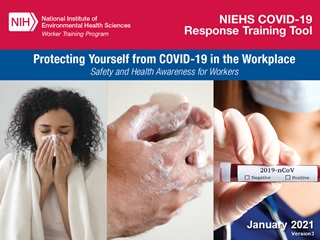
- 1.Protecting Yourself from COVID-19 in the Workplace
- 2.Goal and learning objectives Goal: Increase health and safety awareness for responders and workers with potential exposure to the SARS-CoV-2 virus that causes COVID-19. Learning objectives: After attending participants will be able to: Explain basic facts about SARS-CoV-2 virus. Explain basic facts about COVID-19 disease. Assess the risk of workplace exposure to COVID-19. Define key steps in worker protection and infection prevention and control. Identify methods to prevent and respond to COVID-19 exposure in the workplace. 2
- 3.3 CAUTION! This presentation by itself is not sufficient training for personnel who have potential for occupational exposure to the SARS-CoV-2 virus. Personnel must be trained to their employer’s site-specific policies and procedures. Training must include practice in putting on and taking off PPE and respirators and performing decontamination procedures until competency and confidence can be demonstrated. Caution
- 4.Information on COVID-19 is rapidly changing, sometimes daily. Refer to reliable sources such as the CDC, OSHA, NIOSH, State Health Departments and peer reviewed science publications. 4
- 5.Employer and worker responsibilities Employers and workers have responsibilities under the OSH Act. • The Occupational Safety and Health Act requires that employers provide a safe and healthy workplace free of recognized hazards and follow OSHA standards. • Workers should participate in the development and implementation of the employer’s safety and health policies and help ensure that they are appropriate and implemented. 5 Speak up! You have a right to file a complaint with OSHA, the state or local health department, the mayor, or the police!
- 6.Worldwide distribution map 6 Click the link to see the latest global numbers and numbers by country visit.
- 7.US distribution map 7 Click the link to see the current cases in the U.S.
- 8.Pandemic declaration On March 11, 2020, the World Health Organization (WHO) characterized COVID-19 as a pandemic. It has caused severe illness and death. It features sustained person-to-person spread worldwide. It poses an especially high risk for the elderly (60 or older), people with preexisting health conditions such as high blood pressure, heart disease, lung disease, diabetes, autoimmune disorders, and certain workers. 8
- 9.9 Be informed and prepared. Wear a mask. Maintain social distancing (6 feet). Wash your hands frequently. Use alcohol-based hand sanitizer. Avoid touching your eyes, nose, and mouth. Stay home when you are sick. Cough or sneeze into a tissue or your elbow. Clean and disinfect frequently touched objects and surfaces such as cell phones. What can individuals do?
- 10.Five steps to proper handwashing Wet your hands with clean, running water (warm or cold), turn off the tap, and apply soap. Lather your hands by rubbing them together with the soap. Lather the backs of your hands, between your fingers, and under your nails. Scrub your hands for at least 20 seconds. Need a timer? Hum the “Happy Birthday” song from beginning to end twice. Rinse your hands well under clean, running water. Dry your hands using a clean towel or air dry them. 10
- 11.Precautionary principle When it comes to worker safety, we should be driven by the ‘precautionary principle’ that reasonable steps to reduce risk should not await scientific certainty about the nature of the hazard or risk. 11
- 12.Module 1: COVID-19 Basics 12
- 13.What is SARS-CoV-2? SARS-CoV-2 is the virus that causes coronavirus disease 2019 (COVID-19) SARS = severe acute respiratory distress syndrome Spreads easily person-to-person Little if any immunity in humans Detailed information: https://www.cdc.gov/coronavirus/2019-ncov/index.html 13
- 14.14 Droplet - respiratory secretions from coughing or sneezing landing on mucosal surfaces (nose, mouth, and eyes) Aerosol - a solid particle or liquid droplet suspended in air Contact -Touching something with SARS-2 virus on it and then touching mouth, nose or eyes Other possible routes: Through fecal matter COVID-19 is spread from person to person mainly through coughing, sneezing, and talking and breathing. Transmission
- 15.Incubation period The incubation period is the time between exposure to a virus and the onset of symptoms. With COVID-19, symptoms may show 2-14 days after exposure. CDC indicates that people are most contagious when they are the most symptomatic. Several studies show people may be contagious before developing symptoms. 15
- 16.COVID-19 can cause mild to severe symptoms Most common symptoms include: Fever Cough Shortness of breath Other symptoms may include: Sore throat Runny or stuffy nose Body aches Headache Chills Fatigue Gastrointestinal: diarrhea, nausea Loss of smell and taste 16
- 17.17 Most people will have mild symptoms and should recover at home and NOT go to the hospital or emergency room. Get medical attention immediately if you have: Difficulty breathing or shortness of breath. Persistent pain or pressure in the chest. New confusion or inability to arouse. Bluish lips or face. Severe symptoms – emergency warning signs for COVID-19
- 18.18 A person who has both consistent signs or symptoms and risk factors as follows: What is a person under investigation?
- 19.19 A confirmed case is a suspect case with laboratory-confirmed diagnostic evidence of SARS-CoV-2 virus infection. U.S. Centers for Disease Control and Prevention via AP Confirmed case
- 20.How long does SARS-CoV-2 survive outside of the body? It is not clear yet how long the coronavirus can live on surfaces, but it seems to behave like other coronaviruses. Virus may persist on surfaces for a few hours or up to several days, depending on conditions and the type of surface. It is likely that it can be killed with a simple disinfectant on the EPA registered list below. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2 There are ongoing investigations to learn more. 20
- 21.21 COVID-19 poses a greater risk for severe illness for people with underlying health conditions: Heart disease Lung disease such as asthma Diabetes Suppressed immune systems The elderly have higher rates of severe illness from COVID-19. Children and younger adults have had less severe illness and death. Because COVID-19 is new, there are a lot of scientific unknowns such as the impact on pregnant women and their fetuses. Increased risk of severe illness
- 22.Seasonal flu vs. COVID-19 COVID-19 has the potential to cause more deaths and hospitalizations SARS-CoV-2 is much more infectious and spreads faster than the seasonal flu 22
- 23.Seasonal flu vs. COVID-19 So far, the case fatality rate (CFR) of COVID-19 is estimated to be at around 2%. The CFR of seasonal influenza is estimated to be around 0.1%, making SARS-CoV-2 about 20 times more deadly than the seasonal flu. An estimated 15-20% of infected individuals may suffer from severe symptoms that require medical attention, including pneumonia with shortness of breath and lowered blood oxygen saturation. No Treatment Immunity: unknown how long it will last post illness or vaccination. 23
- 24.24 Flu pandemic fatalities, worldwide, in the last century: 1918 – between 40 and 100 million 1957 – 2 million 1968 – 1 million Experts have been recommending preparedness, warning about the likelihood of future pandemic influenza outbreaks for decades. Pandemic influenza
- 25.Treatment and vaccines In December 2020, the FDA gave emergency use authorization to two COVID-19 vaccines, with many more in the pipeline. There is no specific FDA -Cleared medication or treatment for COVID-19. Treatment is supportive. People who are mildly ill with COVID-19 should isolate at home during their illness. 25
- 26.Module 2: Assessing the Potential for Exposure to COVID-19 in the Workplace 26
- 27.Key exposure factors in the workplace Does the work setting require close contact with people potentially infected with the COVID-19 virus? Do specific job duties require close, repeated or extended contact with people with known or suspected COVID-19? Has the community spread of the virus included cases in the workplace? 27
- 28.28 Examples of work settings health care laboratories autopsy suites Examples of job activities bronchoscopy sputum induction working with specimens in laboratories some dental procedures some autopsy procedures High exposure risk occupations are those working with people with known or suspected COVID-19, especially while performing aerosol generating procedures. High potential for exposure
- 29.29 Examples of work settings hospitals and other types of healthcare facilities medical transport correctional facilities drug treatment centers homeless shelters home health care environmental clean-up of SARS-CoV-2 correctional facilities long term and resident care facilities Examples of job activities direct patient or long term resident care emergency medical services housekeeping and maintenance in patient and resident areas meat packing High potential for exposure
- 30.Medium potential for exposure Examples of work settings Retail stores Public transportation Home visiting occupations Postal and warehouse workers Public services Examples of job activities Stocking shelves Checking out customers Emergency home repairs Handling mail and goods Processing public benefits 30
- 31.Low potential for exposure 31 Low potential for exposure occupations are those that do not require contact with people known to be infected nor frequent contact with the public.
- 32.32 The next few slides will review key considerations for the health care and emergency services industries as well as continuity of operations and the role of public health.
- 33.33 https://www.cdc.gov/coronavirus/2019-ncov/hcp/index.html The CDC site includes guidelines for infection control, EMS, home care, long term care, clinical care, evaluating persons under investigation,and more. Refer to the CDC and state health department guidelines for protection of healthcare workers. In the current and past coronavirus outbreaks, healthcare workers have had a high rate of infection. It is especially important to ensure that procedures, equipment, and training are fully protective. Healthcare settings
- 34.Long term, nursing, and resident care There have been a very large number of COVID-19 cases among resident care workers because of the high prevalence and severity of cases of residents in long term care. Many agencies have guidance for long term care, nursing homes, assisted living facilities, and other resident care facilities. 34
- 35.Emergency services Emergency services and critical infrastructure include: law enforcement fire and EMS hospitals public utilities 35 Emergency services and critical infrastructure must be able to function during a national emergency.
- 36.Healthcare facility identification and isolation The most important steps to prevent spread of COVID-19 Procedures for rapid identification and isolation of suspect COVID-19 cases. Community and hospital procedures to ensure symptomatic people are not in public places, waiting rooms, reception areas, emergency departments, or other common areas Collect a travel history for patients presenting with fever, cough, or shortness of breath. Immediately isolate – using standard, contact, and droplet precautions for suspect or confirmed cases. 36
- 37.Community/workplace connection Examples of work settings schools sports and arts events social services high density of coworkers high contact with the general public including retail and grocery stores Examples of job activities classroom instruction aiding clients serving customers 37 When a community outbreak occurs, any workplace or event location where people gather has a high potential for exposure.
- 38.38 Government Facilities Dams Commercial Facilities Nuclear Power Plants Food and Agriculture Public Health Health care Banking and Finance Chemical Manufacturing and Storage Facilities Defense Industrial Base Water Energy Emergency Services Information Technology Telecommunications Postal and Shipping Transportation Keeping critical infrastructure and key resources operating is a priority! Critical infrastructure
- 39.Continuity of Operations (COOP) All businesses and agencies should have a strategy to overcome potential disruptions to operations for: maintaining critical utilities and infrastructure; rostering personnel with authority and knowledge of functions; policies that enable employees to work remotely; communications with employees and customers, including during disruptions to usual services; stockpiling supplies or developing multiple suppliers in the event of a supply chain disruption. 39
- 40.Role of public health officials Cases reported by employer to local health department to do contact tracing. Investigate contacts of worker who is infected to determine what other cases may be present and to identify potential source. Case identification and containment. Communication and education. Mitigation may include restrictions on public events and gatherings, transportation, and other activities. Promote physical and social distancing and other safety and health measures. 40
- 41.41 Module 3:Methods to Prevent COVID-19 in the Workplace
- 42.42 Preparing for the threat. Implementing preventive measures. Implementing the continuity of operations plan. Managing business recovery post-epidemic. Key steps for preparing for and managing epidemics in the workplace
- 43.Community spread can impact any workplace Mitigation may include shutting down events and worksites where people gather. For example, the National Basketball Association suspended its season on March 11, 2020. Many universities and colleges have suspended in person classes and have moved to distance learning. Workers at stadiums, arts centers, and other places where people gather are impacted. 43
- 44.Consider the impact on workers Will a worker be paid if their workplace shuts down or they are quarantined? What can be done for workers who are sick but have no paid sick leave? How can workers cope with the impact if their child’s school is shut down or their child is placed in quarantine? What can be done for low wage and immigrant workers who have no access to health care? Other impacts? 44
- 45.Stay home when sick. Wear a mask. Wash hands or use sanitizer frequently and after coughing, sneezing, blowing nose, and using the restroom. Avoid touching your nose, mouth, and eyes. Cover coughs and sneezes with tissues or do it in your sleeve. Dispose of tissues in no-touch bins. Avoid close contact with coworkers and customers (6 feet) Avoid shaking hands/wash hands after physical contact with others. 45 Basic hygiene and social distancing
- 46.46 STOP shaking hands!
- 47.Key elements: COVID-19 workplace plan Management leadership and employee participation Hazard identification and assessment Hazard prevention and control Risk communication, education, and training 47 System evaluation and improvement Family preparedness Emergency operations procedures Post pandemic recovery
- 48.Protecting workers 48 Start with the most effective method to protect workers. Physically remove the hazard Replace the hazard Isolate people from the hazard Change the way people work Protect the worker with Personal Protective Equipment
- 49.Engineering controls Ventilation Drive-thru service Plastic shields and other barriers Sneeze guards 49
- 50.Engineering controls for high exposure potential jobs in health care and laboratories Examples include: Negative pressure isolation rooms Biological safety cabinets/HEPA filtration UV irradiation systems 50
- 51.Administrative controls and work practices to reduce exposure Enable sick workers to stay home Establish work from home policy Minimizing contact among workers and clients Discontinue non-essential travel Limiting the number of staff present for high potential exposure tasks Training 51
- 52.Additional administrative controls Soft barriers include use of tables, ropes, signs, and floor markings to maintain social distancing. 52
- 53.Adjust policies to reduce exposures Policies that can help to reduce exposure to COVID-19 include: Encouraging workers who are ill to stay home without fear of reprisals or loss of pay or benefits Using email, phone, teleconferences instead of face-to-face contact 53
- 54.54 Where applicable, the OSHA PPE standard requires employers to: Conduct an assessment for PPE Provide PPE at no cost, appropriate to the hazard Train employees on how to don (put on) and doff (take off) PPE Train workers to maintain, store, and replace PPE Provide medical evaluation and fit testing https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=9777&p_table=STANDARDS OSHA PPE standard
- 55.55 Employers should develop site specific decontamination procedures. Depending on the workplace, decontamination may require consultation with the health department or use of a consultant specializing in environmental cleanup. Use of an EPA registered disinfectant effective is recommended. Worker and building occupant protection is essential to protect against the virus and adverse effects of the disinfectant. EPA List: https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2 Decontamination
- 56.56 An N95 respirator is the minimum level of protection to prevent inhaling coronavirus. Respirators are needed when there is a potential for aerosol transmission. Respirators
- 57.57 Advantages of reusable respirators: Durability Stand up to repeated cleaning & disinfection Maintain fit over time Cost savings Powered air-purifying respirator (PAPR) Half or full-face elastomeric respirators Respirators (continued)
- 58.58 Surgical masks do not: Fit tightly against the skin to form a seal Filter tiny particles, such as viruses or bacteria that are in the air Surgical masks are not respirators! Respirators (continued)
- 59.59 Written program Selection according to hazard Medically fit to wear Fit testing Ensure proper use of respirators Respirator maintenance Labeling/color coding filters Employee training Program evaluation Recordkeeping Respiratory programs must comply with all elements of OSHA Standard 29 CFR 1910.134 Respiratory protection standard
- 60.PPE for jobs with high potential exposure Face/eye protection Gloves Gowns Respirators At least N95 PAPR or full or half face elastomeric for greater protection NOTE: there is a worldwide shortage of PPE! 60
- 61.61 Must be hands-on and frequent Should not be primarily computer based or lecture Must include an opportunity to drill the actual process of donning and doffing PPE and respirators Should include a trained observer Cover site specific decontamination procedures. Training and drills
- 62.Prevention in all work settings Wash hands after removing gloves or when soiled. Wear a mask. Keep common surfaces such as telephones, keyboards clean. Avoid sharing equipment if possible. Minimize group meetings by using phone, email, and avoid close contact when meetings are necessary. Consider telework. Limit unnecessary visitors to the workplace. Maintain your physical and emotional health with rest, diet, exercise, and relaxation. 62
- 63.Protection of essential workers Fire, police, grocery stores, gas stations, utilities, communications, and health care facilities are examples of essential industries and operations that remain open during a pandemic shutdown. A site and job task specific risk assessment should be conducted to document the necessary protective measures. Social distancing measures include use of barriers, signs, modifying work procedures that require close human interaction. Other steps include increased cleaning and disinfection, use of PPE and respirators, and training. 63
- 64.OSHA Hazard Communication standard The hazard communication standard, 29 CFR 1910.1200, establishes a worker’s right to know about chemicals in the workplace Employers are required to develop: List of all hazardous chemicals in the workplace Labels on containers Chemical information (safety data sheets) Training Written program and worker access to information These rights may be relevant to the cleaning and disinfecting of chemicals 64
- 65.Portable containers Portable containers must be labeled Exception: portable containers do not have to be labeled if only the worker who transfers the chemical uses it during that shift 65
- 66.Cal OSHA Aerosol Transmissible Disease (ATD) Standard http://www.dir.ca.gov/Title8/5199.html Enforceable in California, it applies to many types of health care settings, police services, correctional facilities, drug rehab centers, homeless shelters, and other settings. Requires different types of engineering controls, work practices and administrative controls, and PPE depending on the level of potential exposure. It is a useful reference for all states. 66
- 67.Mental health and stress As the number of cases of COVID-19 increase, so does the associated anxiety and stress. Consider the following steps: Use your smart phone to stay connected to family and friends. Shift from texting to voice or video calling to feel more connected. Keep comfortable. Do more of the things you enjoy doing at home. Practice stress relief whenever you feel anxiety building – do some deep breathing, exercise, read, dig in the garden, whatever works for you. Avoid unhealthy behavior such as excess drinking – that will just increase your anxiety afterwards. Keep looking forward. Think about plans you’d like to make down the road. 67
- 68.The Role of the Vaccine Cases of COVID-19 will decrease with the administration of the vaccine. With uptake of the vaccine and continued workplace controls in place, occupational exposures will decrease. People who are vaccinated can still be exposed and potentially expose someone else even if they don’t become sick. A continued focus on maintaining workplace preventive measures is important to protect workers in all industries. 68
- 69.Workers have the right to: Receive workplace safety and health training in a language you understand. Be protected from potentially toxic chemicals like cleaners and disinfectants. Request an OSHA inspection and speak to the inspector. Report an injury or illness and get copies of your occupational medical records. Get copies of the employer’s log of recordable work-related injuries and illnesses. Complaints can be filed by calling 800-321-OSHA or filing an online complaint, as well as in person. Information is available on OSHA’s website at https://www.osha.gov/workers/file-complaint. 69
- 70.PSD Guide The PSD Training Module trains workers how to use existing resources to research and evaluate the characteristics of infectious disease hazards and also to understand the recommended methods for controlling them. 70
- 71.Program design Interactive Adult training techniques Designed for workers & community All hazards approach Structured training materials 71
- 72.Objectives Upon taking this module, participants will be able to: Access and use existing resources for pathogen safety data. Look up key terminology used in pathogen safety data resources. Explain the use of pathogen safety data resources in risk assessment and infection prevention and control activities. 72
- 73.73 PPT presentation Participant worksheet The PSD Guide A glossary Four case studies that can be used as alternative to activities An instructor guide Download the PSD materials: https://tools.niehs.nih.gov/wetp/index.cfm?id=2554 PSD guide training materials
- 74.Acronyms CDC Centers for Disease Control and Prevention EPA U.S. Environmental Protection Agency HEPA high-efficiency particulate air HHS U.S. Department of Health and Human Services JCAHO Joint Commission on Accreditation of Healthcare Organizations LRN Laboratory Response Network NIOSH National Institute for Occupational Safety and Health OSH Act Occupational Safety and Health Act of 1970 OSHA Occupational Safety and Health Administration PAPR Powered air-purifying respirator PPE Personal protective equipment SNS Strategic National Stockpile WHO World Health Organization 74
- 75.For more information Centers for Disease Control and Prevention (CDC) http://www.cdc.gov Occupational Safety and Health Administration (OSHA) http://www.osha.gov World Health Organization http://www.who.int/en/ National Institute for Occupational Safety and Health (NIOSH) http://www.cdc.gov/NIOSH/ NIEHS Worker Training Program https://tools.niehs.nih.gov/wetp/index.cfm?id=2554 75
- 76.Why this training tool was created This training tool was created by the NIEHS National Clearinghouse for Worker Safety and Health Training under a contract (HHSN273201500075U) from the National Institute of Environmental Health Sciences Worker Training Program (WTP). WTP has trained more than 2 million emergency responders and hazardous waste workers since 1987 to do their jobs safely. WTP is a part of the U.S. Department of Health and Human Services, which is a cooperating agency under the Worker Safety and Health Support Annex of the National Response Plan. As part of the coordinated effort, the National Clearinghouse worked with NIEHS, WTP to create this orientation briefing for those who may be exposed to COVID-19 (coronavirus disease 2019). 76
Related